How Stress Affects Your Body: 5 Biological Facts Nobody Tells You
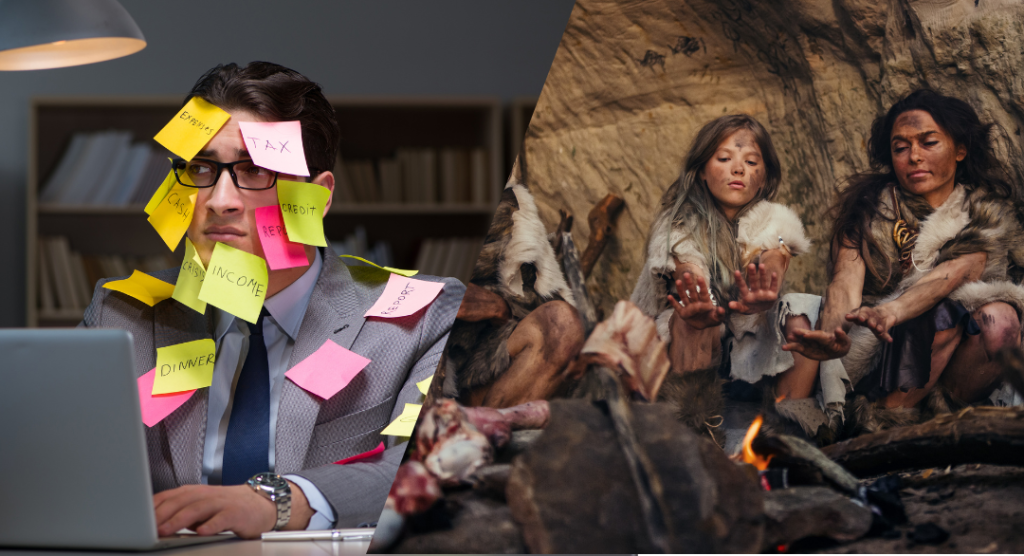
Understanding how stress affects your body starts with a simple truth: your 200,000-year-old survival system can’t tell the difference between a bear attack and a work deadline.
Your heart is racing. Your stomach hurts. You can’t sleep. You’re snapping at people you love. All because of a work project? Seattle traffic? An overdue bill? If you’ve ever wondered how stress affects your body when the threat isn’t actually life-threatening, this article will give you the answers.
The answer lies in an evolutionary mismatch. Your body runs software designed for immediate physical threats—being chased by predators, fighting rival tribes, escaping natural disasters. But today’s stressors are chronic, psychological, and relentless: job insecurity, financial pressure, information overload, social comparison, political anxiety.
At Seattle Wellness Center, clients often express frustration that “normal” daily stress produces such intense physical symptoms. They feel betrayed by their bodies. But here’s the truth: your body isn’t broken. It’s doing exactly what it was designed to do—it just hasn’t evolved to distinguish between a genuine threat and a passive-aggressive email.
This article will help you understand the fascinating biology behind how stress affects your body so profoundly. According to the American Institute of Stress, 75% of Americans report physical or emotional symptoms from stress. Understanding what’s actually happening is the first step toward managing it effectively.
Table of Contents
- The Bear Chase Problem
- What Actually Happens in Your Body
- 5 Ways Chronic Stress Changes Your Body
- The Vicious Cycles That Make Stress Worse
- What Actually Works (And Why)
- When to Get Professional Help
- Frequently Asked Questions
The Bear Chase Problem: Why Your Body Overreacts to Modern Stress
Imagine you’re walking through the forest 200,000 years ago. You hear a twig snap. You turn. A bear is charging toward you.
In that split second, your body launches a remarkable series of changes: your heart pounds to pump blood to your muscles. Your breathing quickens to deliver more oxygen. Your pupils dilate to see better. Blood flow diverts from your digestive system to your legs. Stress hormones flood your bloodstream. Your immune system goes on high alert. Your blood sugar spikes to fuel immediate action.
This is the stress response, also called fight-or-flight. And it’s brilliant. It kept your ancestors alive. The bear scenario would resolve in minutes—you’d escape, fight, or unfortunately become bear food. Either way, the threat would end quickly, and your stress response would shut off.
Now fast-forward to today. Your boss sends a terse email. Your body launches the exact same response. Heart pounding? Check. Stomach in knots? Check. Can’t think clearly? Check. But here’s the problem: there’s no bear to fight or flee from. The threat is psychological, ongoing, and unsolvable by running or punching.
This is the core of how stress affects your body in modern life. According to StatPearls, the stress response evolved to handle acute, short-term threats. When these responses continue for extended periods, they shift from protective to destructive. Your body stays in a state of high alert, constantly preparing for a physical threat that never comes.
🔬 The Numbers Tell the Story
Research from Gallup’s 2023 Global Emotions Report found that 49% of Americans experience significant daily stress—nearly one in two adults. The World Health Organization has identified stress as one of the foremost health crises of the 21st century. Your struggle is not personal failure; it’s a widespread public health issue.
Sources: Frontiers in Psychology 2024
How Stress Affects Your Body: The Biology Explained Simply
To truly understand how stress affects your body, let’s walk through exactly what happens, step by step. This isn’t just academic—knowing the mechanism helps you interrupt it.
Step 1: The Amygdala Sounds the Alarm
According to Harvard Health, the stress response begins in your brain. When you encounter a stressor—whether it’s a bear or a bank statement—your eyes or ears send information to the amygdala, a small almond-shaped structure deep in your brain.
The amygdala is your threat detector. It processes emotional information and decides: is this dangerous? If yes, it hits the panic button before your conscious mind even registers what’s happening. This is why you might feel your body reacting before you’ve fully processed what’s wrong.
Step 2: The HPA Axis Activates
The amygdala sends a distress signal to your hypothalamus, which acts like command central. The hypothalamus activates two systems simultaneously: the sympathetic nervous system (for immediate action) and the HPA axis (hypothalamic-pituitary-adrenal axis) for sustained response.
The sympathetic nervous system triggers release of adrenaline (epinephrine) from your adrenal glands. This is the immediate “get ready NOW” signal. Your heart races, breathing quickens, energy surges through your body.
If the stressor continues, the HPA axis takes over, releasing cortisol—the main stress hormone. Cortisol is more sustained than adrenaline. It keeps your body on high alert, mobilizes energy stores, and suppresses non-essential functions like digestion and reproduction.
Step 3: Your Whole Body Responds
Once cortisol and adrenaline are circulating, changes happen throughout your body:
- Heart and blood vessels: Heart rate and blood pressure increase to deliver oxygen-rich blood where it’s needed
- Lungs: Airways dilate to bring in more oxygen
- Muscles: Blood flow increases to prepare for action; muscles tense
- Liver: Releases stored glucose for quick energy
- Immune system: Shifts to high alert in the short term
- Brain: Sharpens focus on the threat; other thinking becomes difficult
- Digestive system: Slows down (not essential during crisis)
This is all perfectly designed for handling that bear. The problem? This same cascade triggers for non-physical stressors: financial worries, relationship conflicts, work pressure, health anxiety. And unlike a bear encounter, these stressors don’t resolve in minutes.
5 Ways Chronic Stress Affects Your Body: The Biology Behind Physical Symptoms
When stress becomes chronic—meaning it persists for weeks, months, or years—the effects compound. Here’s what research shows about how stress affects your body over time:
1. Your Cardiovascular System Takes a Beating
What happens: Persistent stress keeps blood pressure elevated. Chronic high blood pressure damages blood vessels, promotes plaque formation in arteries, and forces your heart to work harder constantly.
The research: A 2022 study published in JAMA Psychiatry found that individuals experiencing prolonged high stress were two times more likely to develop metabolic syndrome—a cluster of conditions including high blood pressure, high blood sugar, and excess abdominal fat. This significantly increases cardiovascular risk.
What it feels like: Chest tightness, rapid heartbeat even at rest, shortness of breath, feeling like your heart is “working too hard.”
2. Your Immune System Gets Confused
What happens: Short-term stress boosts immunity. But chronic stress suppresses immune function while also promoting inflammation. You become more susceptible to infections and slower to heal, yet your body is in a constant state of inflammation.
The research: According to research in PMC’s review of brain-body stress responses, chronic stress leads to hyper-inflammatory responses that can resemble chronic inflammatory diseases. Prolonged cortisol exposure suppresses protective immune responses while promoting damaging inflammation.
What it feels like: Getting sick more often, wounds healing slowly, mysterious aches and pains, fatigue that doesn’t improve with rest.
3. Your Brain Actually Changes Structure
What happens: Chronic stress physically alters brain structure. Research shows volume changes in areas responsible for memory, emotion regulation, and decision-making. The amygdala (threat detector) becomes hyperactive while the prefrontal cortex (rational thinking) becomes less active.
The research: A comprehensive review in PMC on molecular mechanisms of brain-body communication found that chronic stress is linked to macroscopic changes in brain areas, consisting of volume variations and physical modifications of neuronal networks. These changes contribute to anxiety, depression, and cognitive difficulties.
What it feels like: Difficulty concentrating, memory problems, feeling anxious or depressed, inability to make decisions, constant worry that feels beyond your control.
4. Your Metabolism Goes Haywire
What happens: Cortisol increases appetite (especially for high-calorie foods) and promotes fat storage, particularly around your abdomen. It also affects how your body processes glucose, increasing diabetes risk. Stress literally changes how your body stores and uses energy.
The research: Harvard Health explains that elevated cortisol creates physiological changes meant to replenish energy stores depleted during stress response. But these changes inadvertently contribute to fat accumulation and weight gain. Cortisol increases appetite for energy-dense foods and promotes storage of unused nutrients as fat.
What it feels like: Weight gain despite not eating more, intense cravings for sugar and carbs, difficulty losing weight, feeling like your metabolism has “shut down.”
5. Sleep and Digestion Become Casualties
What happens: Stress disrupts sleep architecture—you have trouble falling asleep, staying asleep, or achieving deep, restorative sleep. Meanwhile, your digestive system, considered “non-essential” during stress, gets neglected. Blood flow diverts away from digestion, enzyme production changes, and gut motility is affected.
The research: According to comprehensive research published in the International Journal of Environmental Research and Public Health, chronic stress affects multiple body systems including respiratory, digestive, and integumentary systems. The connection between stress and digestive issues like IBS is well-documented.
What it feels like: Insomnia, waking up tired even after 8 hours, stomach problems (pain, bloating, diarrhea, constipation), nausea, loss of appetite or stress eating.

The Vicious Cycles: Why Stress Gets Worse Over Time
Understanding how stress affects your body means recognizing how stress creates self-reinforcing cycles. Each problem makes the others worse:
The Stress-Sleep-Stress Cycle
Stress disrupts sleep. Poor sleep makes you more reactive to stress the next day. More reactivity means more stress hormones. More cortisol means worse sleep that night. The cycle intensifies.
The Financial Stress Spiral
Financial stress is the number one stressor for Americans. Financial pressure causes stress, which affects health, which leads to medical bills or missing work, which increases financial strain. The American Institute of Stress notes that people under financial pressure often delay medical care to save money, creating a vicious cycle where stress worsens health and poor health increases financial burden.
The Unhealthy Coping Cycle
Stress drives unhealthy coping mechanisms: overeating, alcohol, smoking, isolation. These provide temporary relief but worsen physical health. Worse health increases stress. More stress drives more unhealthy coping.
Breaking these cycles requires understanding they exist and actively intervening. At Seattle Wellness Center, we help clients identify which cycles they’re caught in and develop strategies to interrupt them.
What Actually Works to Manage Stress (And Why It Works Biologically)
Now that you understand how stress affects your body, let’s talk about evidence-based solutions. These aren’t just “relax more” platitudes—each intervention works through specific biological mechanisms.
1. Exercise: Metabolizing Stress Hormones
How it works biologically: Physical activity literally metabolizes stress hormones. Remember, cortisol and adrenaline were released to fuel physical action. Exercise uses them up the way they were meant to be used. It also stimulates production of endorphins, natural mood elevators.
What research shows: According to the CDC, regular physical activity is one of the most important things you can do for mental health. Even 20-30 minutes daily makes a measurable difference.
Practical application: You don’t need a gym membership. Walk briskly during lunch. Take stairs. Dance in your living room. Movement matters more than intensity.
2. Mindfulness: Interrupting the Amygdala
How it works biologically: Mindfulness practices activate the prefrontal cortex (rational thinking) and calm the amygdala (threat detector). This interrupts the stress response at its source. Regular practice literally rewires stress circuits in the brain.
What research shows: A comprehensive review of over 200 studies on behavioral stress reduction programs found significant outcomes in reducing stress-related health impacts through mindfulness-based interventions.
Practical application: Start with 5 minutes daily. Focus on your breath. Notice when your mind wanders to worries. Gently return attention to breath. This simple practice has profound neurological effects over time.
3. Sleep: Restoring the HPA Axis
How it works biologically: Sleep allows the HPA axis to reset. During deep sleep, cortisol production normalizes, stress hormones clear from your system, and your brain processes emotional experiences from the day.
What research shows: Sleep deprivation amplifies stress reactivity. Getting adequate sleep (7+ hours for adults) is fundamental to stress management, not a luxury.
Practical application: Keep consistent sleep/wake times, even on weekends. Create a wind-down routine. Limit screens before bed. Keep your bedroom cool and dark.
4. Social Connection: Activating the Parasympathetic System
How it works biologically: Positive social interaction activates your parasympathetic nervous system—the “rest and digest” system that counterbalances the stress response. Social support also dampens cortisol release during stressful events.
What research shows: Studies consistently show social support is one of the most protective factors against negative health effects of stress. Isolation amplifies stress impact.
Practical application: Prioritize face-to-face connection. Call a friend. Join a group. Seek community. Quality matters more than quantity.
5. Professional Support: Addressing Root Causes
How it works: Therapy, particularly cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR), helps you identify and change thought patterns that amplify stress, develop effective coping strategies, and address underlying issues contributing to chronic stress.
At Seattle Wellness Center, our therapists (LMHCs and LICSWs) use evidence-based approaches to help you understand your stress response, interrupt harmful cycles, and build resilience. We don’t just teach relaxation techniques—we help you address the root causes and develop sustainable coping strategies.
When to Get Professional Help for Stress
If you’re still wondering how stress affects your body despite trying self-help strategies, it may be time for professional support. Consider reaching out if:
- Stress significantly impairs your work, relationships, or daily functioning
- Physical symptoms persist or worsen (chest pain, digestive issues, chronic pain)
- You’re using unhealthy coping mechanisms (excessive alcohol, substances, overeating)
- You feel hopeless, overwhelmed, or unable to see a way forward
- Sleep problems have become chronic
- You’re experiencing panic attacks or severe anxiety
- You’ve noticed changes in your ability to concentrate or remember things
💙 How Seattle Wellness Center Can Help
Our approach to stress management:
- Understanding first: We help you understand your unique stress response and what’s driving it
- Evidence-based therapy: CBT, MBSR, and other proven approaches
- Address root causes: Not just symptom management, but addressing underlying issues
- Build sustainable skills: Long-term coping strategies, not quick fixes
- Compassionate, non-judgmental: We understand Seattle’s unique stressors (tech culture, cost of living, seasonal affective patterns)
- Flexible scheduling: In-person and telehealth options
📞 Call Seattle Wellness Center: (206) 636-1982
Most major insurance accepted including Premera, Regence, Aetna, and Cigna. Same-week appointments typically available. Serving Seattle and surrounding communities.
Frequently Asked Questions: How Stress Affects Your Body
Why do I feel physical pain when I’m stressed but nothing is physically wrong?
Stress causes real, measurable physical changes in your body—muscle tension, inflammation, altered pain perception, and changes in blood flow. The pain is genuine, not “in your head.” Chronic stress keeps muscles tensed, promotes inflammatory responses, and can lower your pain threshold. This is exactly how stress affects your body physically even when medical tests come back normal. The mind-body connection is real and bidirectional.
Can stress actually cause serious diseases or just make me feel bad?
Yes, chronic stress is a risk factor for serious diseases. Research links prolonged stress to cardiovascular disease, hypertension, diabetes, weakened immune function, and mental health conditions like anxiety and depression. A 2022 JAMA Psychiatry study found that high stress doubled the risk of metabolic syndrome. Stress doesn’t just make you feel bad—it changes your body at the cellular level in ways that increase disease risk.
Why does my stress seem worse than other people’s stress?
Stress response varies significantly between individuals based on genetics, past experiences, current circumstances, support systems, and coping skills. Some people have more reactive stress response systems due to childhood experiences or genetics. Additionally, cumulative stress matters—if you’re dealing with multiple stressors simultaneously (financial + health + relationship issues), the combined effect exceeds the sum of individual stressors. Your struggle is valid regardless of how others handle stress.
How long does it take for my body to recover from chronic stress?
Recovery time varies depending on stress duration and intensity. Acute stress recovery happens in hours to days. For chronic stress lasting months or years, you may notice improvement in weeks (better sleep, less anxiety), but full recovery—including normalization of hormone levels, immune function, and cardiovascular parameters—can take months to a year. The good news: your body is remarkably resilient. With appropriate interventions, healing happens. At Seattle Wellness Center, we help clients track progress and celebrate incremental improvements.
Is it normal to feel stressed all the time in modern life?
While chronic stress has become common (49% of Americans experience daily stress), common doesn’t mean normal or healthy. Your stress response system was designed for intermittent activation, not continuous operation. Chronic stress is a public health crisis, not an inevitable part of modern life. The prevalence of stress-related health problems indicates we need systemic changes in work culture, economic security, and healthcare access—not just individual coping strategies. However, individual interventions can absolutely help while larger systemic changes slowly occur.
Can stress management really make a difference if my stressors aren’t going away?
Yes. While we can’t always eliminate stressors (job pressures, financial realities, health issues), we can change how your body responds to them. Through therapy, mindfulness, exercise, sleep optimization, and other interventions, you can literally rewire your stress response. Two people in identical circumstances can have vastly different physiological responses based on their coping skills and support systems. Stress management isn’t about making problems disappear—it’s about building resilience so your body doesn’t pay such a high price for unavoidable life challenges.
Your Body Isn’t Broken—It Just Needs Support
Now you understand how stress affects your body. The next step is getting the support you need to manage it effectively. Seattle Wellness Center specializes in evidence-based stress management that addresses root causes, not just symptoms.
Monday-Friday 9am-6pm | Same-week appointments available
In-person (Seattle) and telehealth options | Most insurance accepted

About This Resource: This article was created by the licensed therapists (LMHCs and LICSWs) at Seattle Wellness Center to help you understand the biological mechanisms behind stress and its physical effects. We provide evidence-based therapy for stress management, anxiety, and related conditions using approaches like CBT and mindfulness-based stress reduction.
Medical Disclaimer: This article provides educational information and should not replace professional medical or mental health care. If you’re experiencing severe or chronic stress symptoms, please contact Seattle Wellness Center at (206) 636-1982 or consult with healthcare providers. Chronic stress requires professional evaluation and treatment.
Last Updated: February 2026 | Sources: Information based on peer-reviewed research from PMC/NIH, Frontiers in Psychology, American Institute of Stress, StatPearls, JAMA Psychiatry, Harvard Health, CDC, International Journal of Environmental Research and Public Health, and Gallup research. All recommendations reflect current evidence-based practices for stress management.
📞 Seattle Wellness Center: (206) 636-1982
155 NE 100th St Suite 125, Seattle, WA 98125
Serving Seattle and surrounding communities
